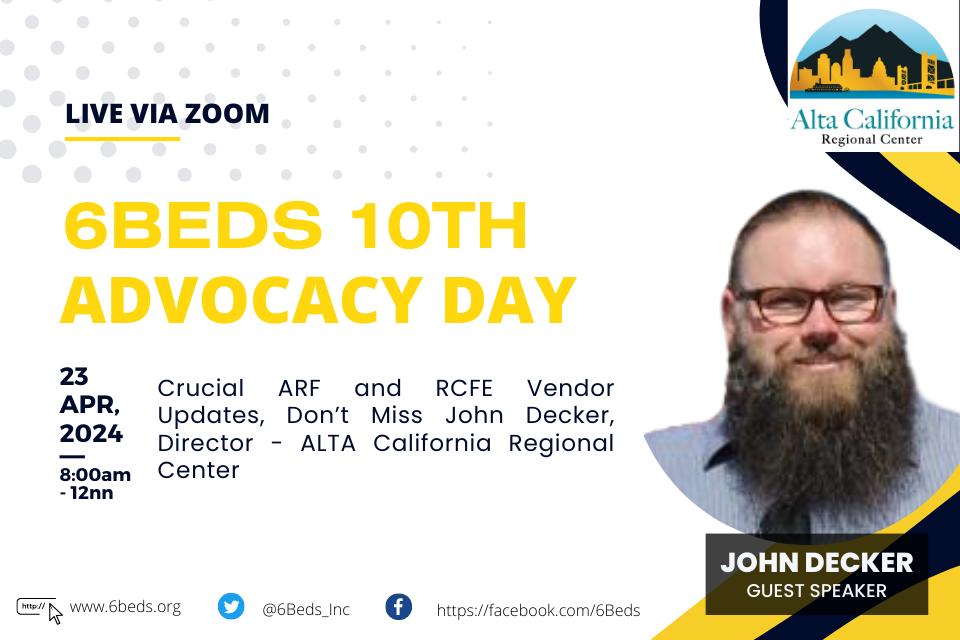
Join John Decker at 6Beds Advocacy Day
A crucial legislative challenge is on the horizon, and your presence is needed more than ever. Join us on April 23 at the 6Beds Advocacy Day to voice your opposition to SB 1406—a bill that could significantly constrain the operations of residential care facilities for the elderly (RCFEs).